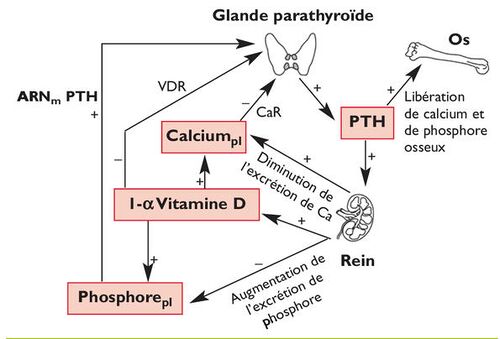
Fonction parathyroïdienne
De médecine.top
Fonction parathyroïdienne
Investigations
- PET-choline
- Scintigraphie parathyroïdienne
Hypoparathyroïdie
- Exclusion d'une hypomagnésémie pouvant causer une hypoparathyroïdie fonctionnelle
Hyperparathyroïdie
Hyperparathyroïdie primaire
- Asymptomatique: suivi à 6−12 mois
- Symptomatique: Guideline-recommended indications for parathyroidectomy include increase in serum calcium level ≥1 mg/dL (0.25 mmol/L) above upper limit of normal; creatinine clearance <60 mL/min, 24-hour urine calcium >400 mg/day (>10 mmol/day), or increased stone risk by biochemical stone risk analysis; presence of nephrolithiasis or nephrocalcinosis by radiograph, ultrasound, or CT; T-score (on DEXA scan) of less than or equal to −2.5 at any site or evidence of vertebral fracture; and age younger than 50 years. Parathyroidectomy is also indicated in patients in whom medical surveillance is neither desired nor possible, and those with complications of hyperparathyroidism including significant bone, kidney, gastrointestinal, or neuromuscular symptoms.
- Vitamin D deficiency is common in patients with primary hyperparathyroidism (HPT) due to increased conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D. Supplementation of vitamin D in patients with HPT has been shown to reduce parathyroid hormone levels, decrease bone turnover, and improve bone mineral density.
Hyperparathyroïdie secondaire
- Etiologie:[1]
- Insuffisance rénale chronique (eGFR <60-30 ml/min)
- Médicaments: biphosphonates, anti-épileptiques, furosémide, phosphore
- Malabsorption ou apports calciques diminués: maladie coeliaque, mucoviscidose, maladie de Crohn, status après bypass gastrique
- Perte rénale de calcium: hypercalciurie rénale
- Insuffisance en vitamine D: 25-OH vitamine D plasmatique <50 nmol/l
- Traitement: calcitriol
Références
MKSAP 18